
Eligibility Verification
Medical Billing Process is captivating its role in the health companies and has different departments to deal with. But are you sure that the income you receive or the staff time you give to your patients are worth enough? This can be assured only when you have proper medical eligibility verification in you billing system.
The very major step practiced by the ones, practicing medical science, is the verification of the medical eligibility of the patients. Insurance companies on a timely occasion alter their policies and programs and it becomes vital to go through the Medical insurance or the health insurance of the patient whenever he comes for the visit. This verification doesn’t let you drown in claims rejections or denials, or the delay of revenue management cycle. We support your billing system keeping “Medical Eligibility Verification” as an important venture.
Verify patient insurance coverage and co-pay amounts up front. Request Demo
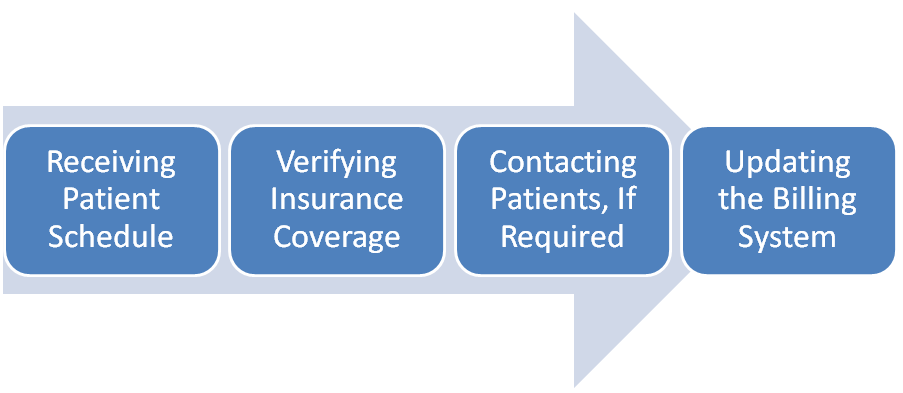
Our Verification Covers Following Process
- Receiving the patient data, details, history of payment and schedule; and to revise them in every appointment.
- Checking of Insurance facts and facets and revising it covering their primary and secondary payers through call. Having a word with their authorized online insurance entrances is required.
- If the eligibility is expired or there are issues regarding the policies, we contact the customer and sort the problem.
- Finally the Billing system is upgraded accordingly with the assertion of member ID, group ID, coverage period, co-pay, deductible and co-insurance information with other benefits.
This verification takes a complete check of the payable benefits, co-pays, deductibles, claims assured, effective date, treatment process, plan rejections and denials, the termination dates, and more.
It helps determining a patient’s financial obligation from information provided by the electronic eligibility response, as to assist you in collection at the point of care.
Your Saving
- The potential saving you get enrich with using electronic eligibility verification states following data:
- Cost of handling paper eligibility verification:
- Cost of handling electronic eligibility verification:
- Average annual savings from electronic eligibility verification per physician:
We, with the help of this process of verification, add much more to your company and read the importance of medical eligibility verification:
- This verification very surely increases the income of your company by avoiding any wastage of money on ineligible patients.
- Besides the advantage of increase in cash collections and reimbursements, it even reduces staff- time by reducing the delays and denials, resulting to better staff efficiency.
- It minimizes errors, reduces bad debts and slow cash collections which promptly supports in reduced operational costs.
- It helps determining a patient’s financial obligation from information provided by the electronic eligibility response, as to assist you in collection at the point of care.
- This insurance eligibility check is just a method to have a more simplified workflow with a good sum of money in hand.
About Us
- 12+ Years of experience
- Certified Medical Billers & Coders
- Completely Familiar with State Guidelines
- Experienced in Software i.e. EHR and etc
- Guaranteed upto 30% increase in revenue.
- Successful track record with multiple speciality.
How it work with 24/7 Medical Billing Services
- 24/7 Medical Billing Services should have the patient information and insurance information before 24-48 hrs of the appointment.
- The team verify the eligibility Verification and the patient eligibility information, Copay, Coinsurance, Deductible before the patient check in.
- Help the practice to collect upfront payment instead waiting for 45-60 days after insurance process and statement sent to patient etc.
- 24/7 Medical Billing Services also work only on Eligibility process for the practice having in-house billing setup.

.png)